After three days packed with high quality clinical presentations, scientific presentations, oral presentations, videos, posters, telecast live surgery, and a fire alarm evacuation thrown in for free, all delegates gathered in the auditorium for the final session of the congress: a summary by six international experts in endometriosis.
It was very interesting to hear their personal views and I felt it was important to invite these six to put pen to paper.
For those actively involved in research, you may find some pointers as to what the experts believe will bring significant change in the next decade.
For those involved in patient care, two well respected surgeons reminded us of the old adage again: “Good surgeons know how to operate. Better surgeons know when to operate. The best surgeons know when not to operate”.
Luk Rombauts
WCE2008 Programme Chair and WES eJournal Editor

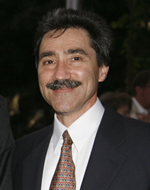
Professor Hans Evers Maastricht University, Netherlands WES President 2008-2011
Micro-RNAs, biomarker studies…clues?
My “personal pearl” of the meeting was the paper presented by Ohlsson Teague from the Adelaide group about the role of micro-RNAs in endometriosis. We all have some 800-1000 micro-RNAs. Every micro-RNA is able to switch off one or more genes. Previous mRNA studies have identified genes that were differentially expressed in eutopic and ectopic endometrium. Not all mRNA levels of proteins known to be elevated in endometriotic tissue differ, however. This suggests post-translational regulation. Micro-RNAs are short single-stranded RNAs that are able to suppress protein expression post-transcriptionally.
This group demonstrated significant differences that exist in the expression of micro-RNAs between eutopic and ectopic endometrium. Not only may this shed new light on the pathophysiology of endometriosis (and on endometrial dysfunction in women with endometriosis), but also could it become a future target for pharmacotherapy by customised drug delivery.
Another striking thing at this meeting were the many biomarker studies, indicating differences between women with endometriosis and women without endometriosis, claiming that a new diagnostic test would soon become available with sensitivities and specificities of up to 100%. These conclusions never stand firm after proper clinical evaluation in an independent second group of patients. In our field of specialty sensitivities and specificities of 75% are not bad at all, so something may come out of these studies eventually, but so far the claims seem to be a little exaggerated.

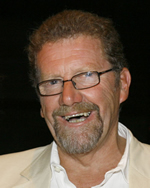
Professor Jacques Donnez University of Louvain, Belgium WES Co-founder and 1st President
Is accreditation for surgery the next step?
First of all, I would like to congratulate the organisers for hosting such a successful meeting, where two parallel sessions, one scientific and one clinical, meant that scientists and clinicians could benefit from the most recent developments in both scientific research and clinical medicine.
This type of meeting was initiated by Professor Evers in Maastricht, where it also proved to be a great success, and I, as founding president, consider that this dual approach must be the rule for all future congresses.
I very much enjoyed the numerous scientific sessions, giving us the opportunity to hear from some of our youngest researchers, most of whom are doing their PhD theses in different labs around the world. They represent what I call the “new blood” of the society.
I was also really impressed with certain moderators who carefully analysed not only their own data, but also data presented by different speakers who came after them.
Having listened to all the new data on angiogenesis and inflammation in endometriosis, I can clearly see the gulf that exists between experimental studies and clinical applications. Scientists and clinicians must continue to work together and share their experience. Scientists need to know what clinicians expect, and clinicians need to know what scientists are able to deliver.
Finally, as a clinician and a surgeon in the field of endometriosis, I have to say that I was disappointed to witness a trend towards aggressive surgery for this benign disease.
We heard lectures on sigmoid resection, we saw videos and live demonstrations but, as I said in my lecture, there is a need for strong and vigorous debate to weigh up the benefits of shaving (debulking surgery) versus rectal resection (radical surgery). Endometriosis is not cancer, but patients want to be free of symptoms.
Conservative surgery means preservation of the blood supply, preservation of the nerves and preservation of the organs. Everything should be done to avoid the high risk of complications (around 10%) encountered after very aggressive surgery.
I would like to ask Bernard Hedon, president of the next congress in 2011, to organise a specific session on this subject. We need to deepen our understanding of this relatively new entity called recto-vaginal nodules or deep endometriosis. We have to analyse the evolution of the disease. But most of all: we need to curb rather than encourage the aggressive approach favoured by some surgeons. Professor Van Caillie gave us a lecture on accreditation. I feel very strongly that we should be accredited not only for surgery itself, but also for the actual decision to proceed with surgery (or otherwise) based on careful analysis of all the indications.

Dr Krina Zondervan Wellcome Trust Centre for Human Genetics, University of Oxford, England
Standardisation and collaboration is the way forward!
WCE 2008 provided, in my opinion, a very successful and stimulating update on ongoing progress in clinical and basic scientific research into a condition that is increasingly recognised as a major public health problem. In particular, state-of-the-art high-throughput technologies in biological analyses present great promise, and, as the meeting showed with some exciting examples, we are starting to witness the application of some of these in endometriosis. An example is the use of proteomic technologies to investigate potential biomarkers for endometriosis, which may in future provide us with a non-invasive diagnostic test.
Genetic studies are likely to tell us, over the next few years, which genes make a woman more or less susceptible to the condition; however, biological studies in blood and tissue will need to show in which biological pathways these genes act in order to identify novel drug targets; epidemiological studies will need to show how such genes interact with environmental factors that are modifiable, and thus open up avenues for prevention.
In this era of exciting new discoveries for many chronic diseases such as diabetes, coronary artery disease, and cancer, we as researchers need to capitalise on pushing for similar research strategies to be adopted for endometriosis.
In order to be successful, however, there is a need for increased adoption of two key concepts in designing future research studies: Standardisation and Collaboration.
Biological studies, such as the proteomic studies mentioned before, have been shown to give highly variable results depending on the experimental protocol adhered to, making comparisons between studies using different protocols virtually impossible.
Furthermore, only large-scale studies will be able to make any progress, and to this end, groups will need to collaborate. No single research group studying small numbers of samples will provide a major breakthrough in a complex condition such as endometriosis. Only through large collaborative studies will sufficient funds be obtained to conduct high-quality research.
Let us enter a new phase in endometriosis research where Collaboration and Standardisation become routine in designing new studies!
Professor Robert Taylor Emory University, Atlanta, USA WES board member
Clinical evolution = good clinical judgment in applying new knowledge
Congratulations should be extended to Prof. David Healy and his team for hosting a highly successful World Congress! The Congress Centre and meeting facilities were excellent, and entertainment at the opening ceremony and congress dinner were wonderful.
WCE 2008 set a record for attendance and the registrants were broadly represented by nationality as well as discipline. Reproductive surgeons, physicians, nurses, embryologists, laboratory scientists, nutritionists, patients and their advocates all contributed openly to a diverse, comprehensive and exceptionally informative program.
As Professor Jacques Donnez observed in his summary of the Congress, the talks and discussion demonstrate a clear evolution in our clinical approach to endometriosis, with more convergence and synergism between surgical and medical treatments.
Nevertheless, he admonished that we must remain prudent in our assessment of new technologies and therapies, and must continue to instil the principles of good clinical judgment in the application of evolving knowledge!
Dr Stephen Kennedy questioned the need for a definitive surgical diagnosis of endometriosis and made a strong case for empirical intervention. From the laboratory and clinical trial perspectives, both new and old drugs are being evaluated for their therapeutic efficacy. During an opening day symposium, progestogens and their multiple pharmacological targets were discussed. Throughout the sessions NF-?B inhibitors, PPAR? ligands and EP2 receptor blockers were entertained as emerging classes of compounds with clinical promise. Natural compounds (eg. catechin) were proposed as novel and potentially safer alternatives to classic pharmaceutical agents. On a more sobering note, Dr Peter Rogers reminded the audience of the potential teratogenic effects of anti-angiogenesis strategies in women of reproductive age.
Professor Hans Evers was impressed by the rapid progress being made in our field by global discovery strategies (eg. cDNA gene expression arrays, multiplexed antibody arrays, proteomics techniques and new investigations into microRNA regulation) and the promise they hold to guide future diagnosis and treatments of women with endometriosis. I too am encouraged by the evolution of our experimental models of endometriosis (cell culture, rodents, and subhuman primates) and advances in the recognition of their advantages and limitations. Methods that began as fundamental mechanism-focused now are being applied to clinically relevant endpoints such as pain and infertility.
Associate Professor Peter Maher Mercy Hospital for Women, Australia President of the International Society for Gynecological Endoscopy
Is endometriosis not a surgical disease after all?
Until WCE 2008 I had always thought of endometriosis as a disease best treated surgically.
Several presenters, in particular in the session on adolescent gynaecology, challenged the unnecessary early intervention with laparoscopy to make the diagnosis before the implementation of medical therapy.
I feel that to leave a conference having learnt one new principle is always worthwhile!
It is important to point out to overseas doctors that most patients, who attend a gynaecologist in Australia, have been investigated and treated by their family practitioner, generally with mediocre results, before referral.
Having said this, there are an increasing number of patients who seek direct referral to a gynaecologist and it is in this group that we should adopt a more conservative medical approach and not perform laparoscopy immediately.
I think that the juxta-positioning of the clinical and scientific sessions at this meeting provided an excellent opportunity for delegates to get the best of both.

Professor Linda Giudice University of California San Francisco (UCSF), USA WES Vice President 2008-2011
Coming full circle: endometriosis is more than just endometriosis
The Xth WCE has been a great success! With nearly 1000 registrants, the meeting brought together clinicians, scientists, pharma, patient advocates, and many, many trainees – all with the goal of understanding, diagnosing, preventing, treating, and curing endometriosis.
The key note speakers gave state of the art addresses, educating us all, and the session formats were highly successful, with having a leader in the field giving a summary presentation of relevance for the session’s free communications. Finally, the debates were provocative and informative.
With regard to aetiology, genetics and the environment took the lead as contenders for the development of endometriosis. In addition, the meeting brought infection as a potential cause, including E Coli and HPV.
Several free communications and key note addresses underscored the diversity of mechanisms and systems involved in the pathophysiology of the disorder, including, eg. progesterone-resistance, stem/progenitor cells, inflammation and the immune system, the role of angiogenesis and lymphangiogenesis, leptin, and micro RNAs.
It is increasingly clear that endometriosis is a spectrum of several distinct types of disease – peritoneal, deep infiltrating, ovarian endometriomas, and extra-pelvic disease. Exciting new data were presented on nerve bundles present in greater density in myometrium, basalis, and functionalis of women with versus without endometriosis, with hormonal dependence of their density observed. In addition, nerve fibres are present only in functionalis of women with disease, as well as in endometriotic foci. The physiologic relevance of this is yet to be determined, although this is a major step forward to understand pain associated with endometriosis.
It was the consensus of the meeting, including patients, investigators, and clinicians, that a diagnostic for endometriosis is a “must do”. Exciting data were presented on proteomics and genomics, and the hope is that this will be a reality as a commercialised entity within the next two to five years.
Overall, from the scientific perspective, this meeting was the prototype for systems biology – translational research with teams of clinicians, scientists, biostatisticians, bionformaticians, epidemiologists, and patients.
We have come full circle to address endometriosis, and the future is in the hands of our young, curious, and energetic trainees and our multidisciplinary teams, closely aligned with our patients. There is a future for young clinicians and scientists and a tremendous opportunity to do well by women with endometriosis – to prevent, treat, and hopefully cure this enigmatic disorder that bears heavily upon the well being of women and their families and friends.
It augurs well for the future of our disciplines that so many capable individuals are committed to ameliorating and ultimately eliminating endometriosis as a cause of pain and disability for women.