The international Pelvic Pain Society held the 3rd World Congress Meeting on Abdominal and Pelvic Pain in Washington on 12-15 October, 2017. Three keynote speakers presented research, implications for treatment, and other avenues to consider when looking at women with endometriosis.
Keynote speakers included Stacey Missmer, professor of obstetrics, gynaecology, and reproductive biology at Michigan State University; Katy Vincent, senior pain fellow in the Nuffield Department of Obstetrics and Gynaecology at the University of Oxford; and professor Robert Taylor of the Wake Forest School of Medicine in North Carolina.

Professor Stacey Missmer
Mitchigan State University
According to Stacey Missmer, research in endometriosis is focused on the onset in early adulthood with very little research looking at adolescence. Many of those experiencing endometriosis-like symptoms see a primary care physician, are prescribed oral contraceptives, and then have success in symptom reduction.
This success is likely due to the oral contraceptive pill, but endometriosis is never clearly diagnosed because the symptoms have resolved and are hard to capture in research.
We don’t know if these women differ in pathology and symptoms, and knowing that could change diagnosis of endometriosis and possible interventions after more research,
states Missmer.
Pain processing
The pain experience of women with a confirmed diagnosis of endometriosis impacts the nervous system both centrally and peripherally. Recent research has shown evidence of central changes associated with dysmenorrhoea (1) alone, and these implications could be overlaid in endometriosis.
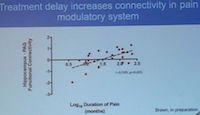 Katy Vincent expands on how this impact occurs, including repeated episodes of pain, psychological distress, the location of nerve fibres in inflammation, dysfunction of the HPA axis, and comorbid pain conditions. These comorbid pain conditions increase the burden of the pain experience and influence of symptoms and amplifying pain. In patients with endometriosis, excitatory neurotransmitter levels are increased which facilitates conduction along pain-modulatory pathways (2).
Katy Vincent expands on how this impact occurs, including repeated episodes of pain, psychological distress, the location of nerve fibres in inflammation, dysfunction of the HPA axis, and comorbid pain conditions. These comorbid pain conditions increase the burden of the pain experience and influence of symptoms and amplifying pain. In patients with endometriosis, excitatory neurotransmitter levels are increased which facilitates conduction along pain-modulatory pathways (2).
The amount of connections in this modulatory system increases in relation to the length of time a woman experiences pain; we need to be treating pain symptoms earlier before we even begin to think about the cause.
Central Pain
 Nerves conducting these pain signals through the central network can lead to an increase in neuropathic input and decreased nociception as the nerves are in close proximity to inflammation (3,4). This process occurs following surgery indicating ‘further harm may be occurring by performing repeat surgeries in this patient population’. Central pathways maintain the neuropathic pain state generated from inflammation, leading to further amplification of pain (5). Aside from the science of pain processing, we must consider the comorbidities of endometriosis and how they affect women.
Nerves conducting these pain signals through the central network can lead to an increase in neuropathic input and decreased nociception as the nerves are in close proximity to inflammation (3,4). This process occurs following surgery indicating ‘further harm may be occurring by performing repeat surgeries in this patient population’. Central pathways maintain the neuropathic pain state generated from inflammation, leading to further amplification of pain (5). Aside from the science of pain processing, we must consider the comorbidities of endometriosis and how they affect women.
There is increasing evidence that central factors are just as important for chronic abdominal and pelvic pain as other factors but there is not yet enough knowledge on effective interventions. We are learning these central concepts to pain are important; not just the peripheral concepts to pain.
said Vincent.
Psychological influence
Psychological alterations occur in many women with endometriosis and these comorbidities can also amplify or influence the pain experience. Ploghaus’ research shows anxiety amplifies the pain experience (6), but more depressive symptoms have been shown to interrupt the brain centres regulating emotion in relation in pain (7).
Peripheral pain
 Pain associated with endometriosis also involves peripheral nerves and this pain has been shown to involve the immune response system.
Pain associated with endometriosis also involves peripheral nerves and this pain has been shown to involve the immune response system.
Research by Ryan and Taylor shows increased IL-1β (Interleukin -1β) stimulated by endometriotic implant growth due to activation of macrophages (8). Immune cells grow into the endometriotic lesions and then play a role in endometriosis-associated pain (8).
Endometriotic cells in the pelvis recruit these immune cells which generates a signal that stimulates growth of blood vessels and nerves throughout the surrounding tissue,
states Robert Taylor.
Taylor touched on an unpublished study performed by Yu et al, which showed immune cells were attracted to endometriotic lesions by inflammatory mediators (cytokines, growth factors, and prostaglandins). In this process, these mediators activated Brain Derived Neurotrophic Factor (BDNF) or caused an up-regulation of this protein. The up-regulation of BDNF led to further stimulation of blood vessel and nerve growth throughout the afferent pathways leading to increased neuro-angiogenesis and pain (pelvic pain) (9).
The (IL-1β-NF-ҝB-BNDF) pathway serves as an exemplar of nociceptive signalling in endometriosis,
summarises Taylor. A study by Miller et al suggests there are NF-ҝB (nuclear factor kappa light chain enhancer of activated B cells) inhibitory drugs that could be repurposed to modulate the activity along these nociceptive pathways (10). Additionally, Taylor mentions natural herbal chemotherapeutics, such as curcumin and lycopene, that may have an inhibitory effect on the NF-ҝB action.
Dr Lorimer Moseley illustrated the concept by describing the body as a machine and a garden:
What happens on one side of the body, or the garden, affects other areas.
To influence the pain burden experienced by patients, including those with endometriosis, a conceptual change needs to occur when addressing the more central factors. For this change to occur the concept must first be identified and then a plan for conceptual change should be made. Whatever the intervention that goes along with conceptual change the change ultimately occurs because other concepts are made more dominant within the brain and pain pathways. Intervention options can be created for the patient but there are some already created and effective resources available such as tamethebeast.org, the Pain Coach Application, and eCentre Clinic. Once a plan is in place, it is important to recognise it will take time for change to occur within the patient but it can happen. The evidence and information presented by Dr Moseley addresses the whole person.
Conclusion
All of the research and insights on pain processing and how they affect or are altered in women with endometriosis ultimately validate the experience of these women, including the symptoms that seemingly have no ’identifiable source‘. As Vincent explains:
believe your patient… there is still a lot we don’t know.
References
- Vincent K, Warnaby C, Stagg C, Moore J, Kennedy S, Tracey I. Dysmenorrhoea is associated with central changes in otherwise healthy women. Pain 2011;152(9):1966-1975.
- As-Sanie S. Sawsan (Suzie). Pain mechanisms in endometriosis: understanding the neurobiology of chronic pain to enhance patient care. Endometriosis Foundation of America. 2017 [cited 25 October 2017].
- Von Hehn C, Baron R, Woolf C. Deconstructing the Neuropathic Pain Phenotype to Reveal Neural Mechanisms. Neuron 2012;73(4):638-652.
- Neziri A, Bersinger N, Andersen O, Arendt-Nielsen L, Mueller M, Curatolo M. Correlation Between Altered Central Pain Processing and Concentration of Peritoneal Fluid Inflammatory Cytokines in Endometriosis Patients With Chronic Pelvic Pain. Regional Anesthesia and Pain Medicine 2014;39(3):181-184.
- Millan MJ. Descending Control of Pain. Progress in Neurobiology 2002 Apr;66(6):355-474.
- PloghausA, Narain C, Beckmann CF, Clare S, Bantick S, Wise R, Matthews PM, Rawlins JN, Tracey I. Exacerbation of Pain by Anxiety is Associated with Activity in a Hippocampal Network. Journal of Neuroscience 2001;21(24):9896-903.
- Berna C, Leknes S, Holmes EA, Edwards RR, Goodwin GM, Tracey I. Induction of Depressed Mood Disrupts Emotion Regulation Neurocircuitry and Enhances Pain Unpleasantness. Biological Psychiatry 2010; 67(11):1083-90.
- Ryan IP, Taylor RN. Endometriosis and Infertility: New Concepts. Obstetrical and Gynecological Survey 1997;52(6):365-71.
- Wessels JM, Kay VR, Leyland NA, Agarwal SK, Foster WG. Assessing Brain-Derived Neurotrophic Factor As a Novel Clinical Marker of Endometriosis. Fertility and Sterility 2016;105(1):119-28.
- Miller SC, Huang R, Sakamuru S, Shukla S, Matia AR, Shinn P, Van Leer D, Leister W, Austin CP, Xia M. Identification of Known Drugs that Act as Inhibitors of NF-ҝB Signaling and Their Mechanism of Action. Biochemical Pharmacology 2010;79(9):1272-1280.
About the author

Brittany Gosse
Medical Associates Clinic and Health Plans, Dubuque, USA
Brittany Gosse received her Doctorate of Physical Therapy from Clarke University in 2016. She has worked at Sullivan Physical Therapy in Austin (TX), USA, an all pelvic health speciality physical therapy clinic. Britt currently works at Medical Associates Clinic and Health Plans in Dubuque (IA), USA, leading development of a pelvic health physical therapy program. Britt treats orthopaedic and pelvic health conditions with 2,000+ hours of experience in pelvic conditions, including those diagnosed with endometriosis. She is a member of the World Endometriosis Society, International Pelvic Pain Society, and International Society for Study of Women’s Sexual Health. Her interest in endometriosis began with a diagnosis of her own.
